Ankylosing Spondylitis
Overview of Ankylosing Spondylitis
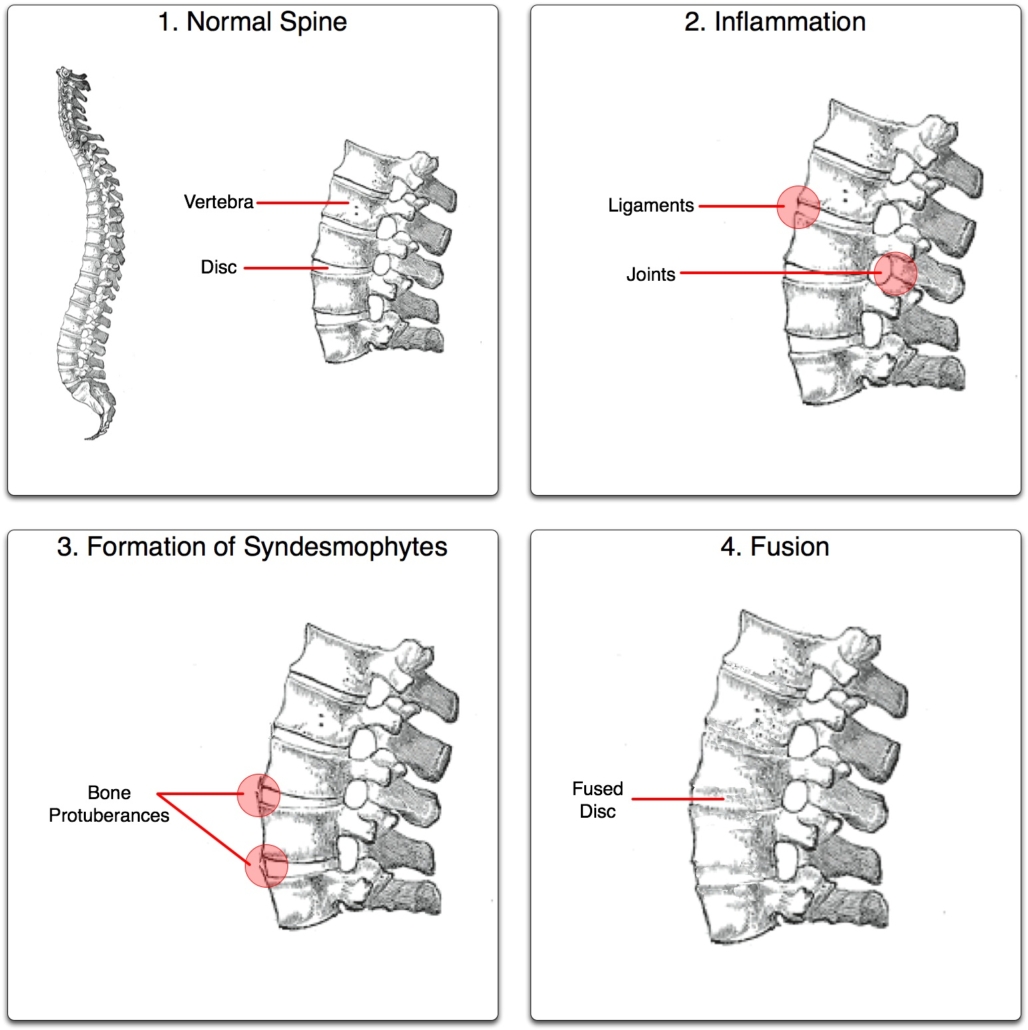
Ankylosing Spondylitis (AS) belongs to a group of types of arthritis known as “spondyloarthritis”. Spondyloarthritis primarily causes inflammation in the joints of the spine. Interestingly, Ankylosing Spondylitis affects about 1 in 200 people. It is a long-term disease that causes inflammation and pain in the spine and can potentially lead to the spinal vertebrae fusing together.
Types of Spondyloarthritis
Although Ankylosing Spondylitis is a type of spondyloarthritis, there are other types found as well. While they all share most symptoms, they target different areas of the body. Other types include:
• Enteropathic arthritis, which is linked to gut inflammations.
• Psoriatic arthritis, related to the skin condition psoriasis.
• Reactive arthritis, which usually follows an infection.
• Undifferentiated spondyloarthritis, where symptoms don’t fit any other type.
Causes of Ankylosing Spondylitis
The exact cause of AS is unknown. However, scientists believe it likely involves genetic factors. Most people with AS have a gene known as HLA-B27, but not everyone with this gene develops the condition. Research also suggests that environmental factors – like gastrointestinal infections – might interact with genes to trigger AS.
Symptoms of Ankylosing Spondylitis
Some people experience mild discomfort, while others have severe, continuous pain. Common symptoms include:
• Chronic, dull pain and stiffness in the lower back or buttocks.
• Difficulty with standing or walking due to spinal stiffness.
• Pain and swelling in other parts of the body, like the shoulders, hips, ribs, feet, and hands.
• Fatigue or tiredness.
• Some people also have bowel inflammation, eye inflammation, heart problems, or lung problems.
Diagnosis of Ankylosing Spondylitis
A primary care doctor or a rheumatologist can diagnose AS. Diagnosis involves:
• Patient medical history review, including symptoms and family history of AS.
• Physical examination to check for pain and mobility in the spine.
• Blood tests to look for inflammation.
• Imaging tests such as X-rays or MRIs to look for changes in the joints and bones.
Treatment Options for Ankylosing Spondylitis
While there’s no cure for AS, treatments can alleviate symptoms and possibly slow disease progress. These include:
• Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), which reduce inflammation and pain.
• Disease-Modifying Anti-Rheumatic Drugs (DMARDs), which can slow disease progression.
• Physical therapy, helping maintain flexibility and improve posture.
• Surgery, in severe cases, to help improve posture or replace damaged joints.
Living with Ankylosing Spondylitis
Living with AS can be challenging. However, certain lifestyle changes can help manage the symptoms effectively:
• Regular exercise, like swimming or walking, helps keep the spine flexible.
• Maintain good posture, like standing and sitting straight.
• Stay hydrated and maintain a healthy diet.
• Quit smoking as it can exacerbate the symptoms.
• Certain relaxation techniques, like yoga or mindfulness, can help manage pain and stress related to AS.
When to Seek Help
If you exhibit early signs of AS, it’s essential to seek help immediately as early diagnosis and treatment can significantly increase your quality of life. Seek help if you experience prolonged pain in any joint, neck/back pain and stiffness that are worse in the morning, discomfort that is relieved by exercise, fatigue or if you have a family history of AS. Contact your doctor instantly if your symptoms worsen or you develop new symptoms, like fever, loss of appetite, or pain in the eyes.
Ensure you engage in regular follow-ups with your healthcare provider and report any changes in your condition promptly. Managing AS is a lifelong commitment, but with a well-balanced treatment plan, it’s possible to lead an active and fulfilling life.
