Lumbar Disc Herniation
Overview
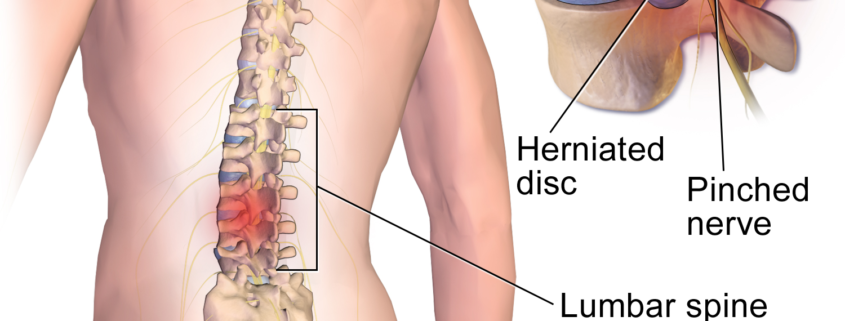
Lumbar disc herniation, commonly referred to as a slipped or ruptured disc, is a prevalent condition affecting back health. It happens when the soft jelly-like center of a spinal disc pushes through a tear in the tougher exterior. The condition predominantly occurs in the lower back, also known as the lumbar spine, which can irritate nearby nerves, resulting in pain, numbness, or weakness in an arm or leg.
Types
While all disc herniations involve a disruption of the disc’s outer ring and irritation of the surrounding nerves, some variations get specially categorized depending upon their location:
1. Posterior herniated disc: Opening toward the back of the spine, this is the most common disc herniation noticed.
2. Anterior herniated disc: This type is quite rare, where the disc ruptures toward the abdomen.
3. Far lateral herniated disc: Opening on the side of the vertebra, this represents about 10% of all observed herniated discs.
Causes
Lumbar disc herniation predominantly results from the natural, age-related wear and tear called disc degeneration. As we age, our spinal discs lose some of their water content, becoming less flexible and more prone to tearing or rupturing. Common causes or risk factors often include:
– Aging
– Improper lifting of heavy items
– Excessive body weight
– Sedentary lifestyle
– Repetitive activities that stress the spine
Symptoms
Symptoms of Lumbar disc herniation may vary but commonly include:
– Pain and numbness, typically on one side of the body that intensifies at night or with certain movements.
– Weakness in the muscles served by the affected nerves.
– Tingling or burning sensation in the affected area.
– Pain that travels down your legs, usually extending to the calf or foot.
Diagnosis
Diagnosis of Lumbar Disc Herniation typically involves a physical examination during which your doctor will check for the source of pain. Clinical tests that might be performed include:
– MRI or CT scan: These imaging tests help to give a detailed view of the herniated disc.
– Nerve tests: Electromyographies or nerve conduction studies may be used to measure electrical impulses in the nerves.
Treatment Options
Several treatment options exist for Lumbar disc herniation, ranging from conservative therapy to surgical intervention. The choice of treatment will typically depend on the severity of symptoms:
Conservative treatments generally include:
– Over-the-counter pain medications
– Physical therapy or a customized exercise program
– Steroid injections to reduce inflammation
Surgical treatments may be considered if conservative treatments prove ineffective or if the patient is experiencing severe symptoms:
– Discectomy: Removes the damaged portion of the disc.
– Spinal fusion: Involves the fusion of vertebrae to provide stability to the spine.
Living With Lumbar Disc Herniation
Proper management and lifestyle changes are key to living with lumbar disc herniation. These may include:
– Regular exercise: Gentle exercises such as walking or yoga can improve flexibility and strength.
– Weight management: Maintaining a healthy weight can reduce pressure on the lumbar spine.
– Good posture: Proper body mechanics during daily tasks can minimize strain on the back.
When to Seek Help
It is essential to seek emergency medical attention if you experience:
– Severe pain that does not improve with rest.
– Sudden weakness or numbness in both legs.
– Loss of bowel or bladder control.
– Trouble walking or standing due to pain.
Lumbar disc herniation is a common and usually manageable condition. By understanding your condition, incorporating lifestyle changes, and taking approved medication or treatment, you can manage symptoms effectively and lead a balanced life. As with any medical condition, always consult with a healthcare professional to explore the best treatment options for your individual situation.
