Osteoarthritis of the Acromioclavicular Joint
Overview of Osteoarthritis of the Acromioclavicular Joint
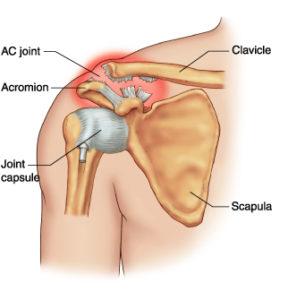
Osteoarthritis of the acromioclavicular (AC) joint, also known as acromioclavicular arthritis, affects the joint at the top of your shoulder where your collarbone and shoulder blade meet. This condition is common and is often a result of aging or overuse. It is characterized by the breakdown and eventual loss of the cartilage of one or more joints.
Causes and Risk Factors of AC Joint Arthritis
Osteoarthritis occurs as a result of the progressive wear and tear of the joint. This is influenced by factors such as:
-
- Age: The risk of developing AC joint osteoarthritis increases with age.
-
- Gender: Although it affects both genders, men are more likely to develop it especially after the age of 40.
-
- Physical activity: It is common amongst people who engage in activities involving repetitive shoulder motion such as weightlifting.
-
- Injury or trauma: Previous injury or trauma to the AC joint makes it more susceptible to osteoarthritis.
-
- Familial predisposition: There may be a genetic component as it often runs in families.
Symptoms of AC Joint Osteoarthritis
Identifying symptoms of AC joint osteoarthritis can be the first step to seeking treatment. Common symptoms include:
-
- Pain and tenderness in the shoulder.
-
- Difficulty moving the shoulder, especially overhead movements.
-
- A popping or clicking sound during movement.
-
- Pain that worsens with activity and relieves with rest.
Diagnosis of Osteoarthritis of the Acromioclavicular Joint
Doctors typically diagnose AC joint arthritis based on a combination of medical history, physical examination, and imaging tests. During the examination, your doctor will assess the range of motion in your shoulder and the level of pain during certain movements. Imaging tests such as X-rays or MRI scans can provide a clearer picture of the joint and confirm the diagnosis.
Treatment Options
Treatment for AC joint osteoarthritis generally involves a combination of non-surgical and surgical options.
Non-surgical treatments:
-
- Physical therapy: Beneficial in improving shoulder strength and flexibility.
-
- Pain medication: Over-the-counter pain relievers and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and swelling.
-
- Rest and activity modification: Limitation of activities that exacerbate the pain.
-
- Steroid injections: Can provide temporary relief of symptoms
Surgical treatments:
If non-surgical treatments do not provide relief, surgical intervention can be considered. The goal of surgery is usually to remove the arthritic part of the joint, which can often be done through minimally invasive arthroscopic surgery.
Living With Osteoarthritis of the Acromioclavicular Joint
Living with chronic shoulder pain can be challenging, but it is often manageable with medication, physical therapy, and lifestyle modifications. Regular exercise can help maintain range of motion and strengthen surrounding muscles. Maintaining a healthy weight can reduce stress on the joint. Heat or cold therapy can relieve inflammation and pain.
When to Seek Help
It’s important to seek medical help if you have persistent, worsening shoulder pain that interrupts your daily activities or sleep and doesn’t improve with self-care measures. Severe joint swelling, sudden loss of function, or inability to move the joint may indicate a more serious problem that needs immediate attention.
