Plantar Fasciitis
Overview
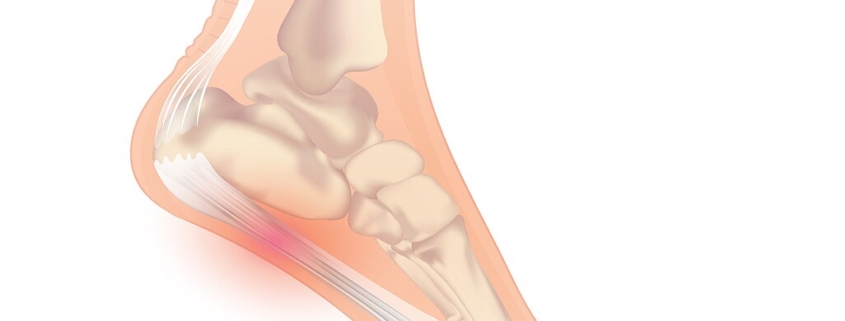
Plantar Fasciitis is a common, and often painful, condition that affects a significant percent of the adult population. Frequently experienced by athletes and individuals who stand for long periods, plantar Fasciitis typically presents pain and stiffness in the bottom (or plantar surface) of the heel.
This condition is caused by inflammation of the plantar fascia – a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. The discomfort caused by this condition can range from a dull ache to a sharp, stabbing pain, often felt upon taking the first steps in the morning or after a long period of rest.
Types
Although plantar Fasciitis is a very specific condition, the experiences of those living with it can greatly differ. Some may experience symptoms constantly, while others may have bouts of pain interleaved with symptom-free periods. One way of categorizing this condition is by its severity, splitting into three categories: mild, moderate, and severe plantar Fasciitis.
Causes
Plantar Fasciitis arises due to strain on your plantar fascia, leading to tiny tears on the surface and causing it to become inflamed. Risk factors include:
-
- Age: Most common between the ages of 40 and 60.
-
- Certain kinds of exercise: Activities that place a lot of stress on your heel and attached tissue such as long-distance running, dancing or ballet, can contribute to an onset of plantar fasciitis.
-
- Foot mechanics: Flat feet, a high arch or an unusual pattern of walking can affect the way weight is distributed when you’re standing and can put added stress on the plantar fascia.
-
- Obesity: Excess pounds put more stress on your plantar fascia.
-
- Occupation: Jobs that keep you on your feet or involve strenuous activity can cause plantar fasciitis.
Symptoms
The main symptom of this condition is pain on the bottom of your foot, around your heel and arch. It can range from a dull ache to a sharp pain, particularly experienced:
-
- Upon first steps in the morning.
-
- When standing up after sitting for a while.
-
- After (not during) exercise.
Some people may also have swelling in their foot.
Diagnosis
Diagnosis of plantar Fasciitis is based on your medical history and a physical examination by a healthcare provider. There’s usually no need for X-rays or other diagnostic tests, unless there’s suspicion of another underlying condition causing the pain.
Treatment Options
Treatment of plantar Fasciitis focuses on relieving pain and reducing inflammation. Options include:
-
- Physical therapy: Stretching exercises and other physical activities can help ease the pain and help with recovery.
-
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended for short-term relief of pain and inflammation.
-
- Surgery: In severe cases or when conservative treatments don’t help, surgery might be considered. This is a last-resort treatment and is rarely needed.
Living With Plantar Fasciitis
Lifestyle changes and coping strategies can make a big difference in managing this condition:
-
- Regular stretching: Keeping the foot, calf and achilles tendon flexible can help reduce pressure on the plantar fascia.
-
- Exercise: Regular exercise can help maintain a healthy weight, reducing stress on the plantar fascia.
-
- Comfortable footwear: Wear shoes with good support and cushioning. Avoid walking barefoot, which can put strain on the fascia.
When to Seek Help
It’s important to seek medical help if your foot pain is persistent, especially if it affects your ability to walk or do daily activities. Sudden, severe foot pain, swelling or difficulty walking after injury could be a sign of more serious issues and should be addressed immediately by a healthcare provider.
Remember, it’s crucial to listen to your body and seek professional advice when needed. You don’t have to live with pain – treatments are available, and they can significantly improve your quality of life.
