5 Essential Questions to Ask Your MSK Specialist
Navigating the world of musculoskeletal (MSK) health can be a daunting task, especially when faced with complex conditions or persistent pain. Whether you’re seeking relief from joint discomfort, muscle strains, or chronic conditions, having a productive conversation with your MSK specialist is crucial.To help you make the most of your appointment, we’ve compiled a list of 5 essential questions that will not only empower you to take charge of your health but also deepen your understanding of your condition and treatment options. By the end of this listicle, you’ll be equipped with the knowledge to engage meaningfully with your specialist, ensuring that your concerns are addressed and your path to recovery is clear. Let’s dive in and explore these pivotal questions that can pave the way for a healthier, more informed you!
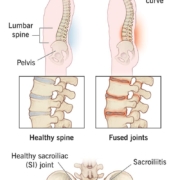
1) What specific diagnosis do you believe is causing my symptoms, and how did you arrive at this conclusion? Understanding the root cause of your musculoskeletal issues is crucial for effective treatment
Understanding the specific diagnosis behind your musculoskeletal symptoms is vital for tailoring an effective treatment plan. When you ask your specialist about this, they should provide a clear clarification of their thought process. This may include a combination of clinical evaluations, imaging studies, and patient history. Effective communication of their reasoning can definitely help demystify the complexities of your condition and empower you to take an active role in your recovery. Consider the following factors they might discuss:
- Symptom Analysis: How your symptoms present and evolve over time.
- Physical Examination: Findings from hands-on assessments of strength, mobility, and pain levels.
- Diagnostic Imaging: Results from X-rays, MRIs, or CT scans that reveal structural issues.
- Laboratory Tests: Blood tests that can rule out inflammatory or autoimmune conditions.
Onc they articulate the diagnosis, it’s essential to delve deeper into how they arrived at this conclusion. This not only builds trust but also enhances your understanding of the treatment journey ahead. A well-rounded approach may involve discussing:
| Method | Purpose |
|---|---|
| Clinical assessment | To evaluate functional limitations and pain triggers. |
| Imaging Techniques | To visualize underlying anatomical issues. |
| patient History | To identify patterns and potential risk factors. |
By engaging in this dialog,you ensure that both you and your specialist are on the same page,paving the way for a more focused and effective treatment strategy.Understanding the rationale behind your diagnosis not only clarifies the path forward but also fosters a collaborative relationship with your healthcare provider.
2) What are the available treatment options for my condition, and what are the potential risks and benefits associated with each? Having a clear view of your choices empowers you to make informed decisions about your health
When discussing treatment options for your musculoskeletal condition, it’s essential to explore a variety of avenues. Potential treatments may include:
- Physical Therapy: Aimed at improving mobility and strength, physical therapy can enhance recovery and reduce pain. Though, it requires commitment and may take time to show results.
- Medications: Anti-inflammatory drugs or pain relievers can provide immediate relief. Be aware of potential side effects, such as gastrointestinal issues or dependency.
- Surgery: In some cases, surgical intervention may be necessary to correct structural problems. While this can lead to significant advancement, it also carries risks like infection or prolonged recovery.
- Alternative Therapies: Options like acupuncture or chiropractic care may offer relief for some individuals. Though, the efficacy can vary, and it’s crucial to ensure practitioners are licensed and reputable.
Understanding the potential risks and benefits associated with each treatment can empower your decision-making process. below is a simple overview of these factors:
| treatment Option | Benefits | Risks |
|---|---|---|
| Physical Therapy | Improves strength and mobility | Time commitment required |
| Medications | Immediate pain relief | Possible side effects |
| Surgery | Corrects structural issues | Risk of complications |
| Alternative Therapies | Holistic approach to pain | Varied effectiveness |
3) How long should I expect the treatment process to take,and what kind of outcomes can I realistically anticipate? Setting proper expectations can definitely help you stay motivated and engaged throughout your recovery journey
Understanding the timeline of your treatment process is crucial for maintaining motivation and engagement throughout your recovery journey. Generally, the duration of treatment can vary significantly depending on several factors, including the specific condition being addressed, the chosen treatment method, and your individual response to therapy. Here are some key points to consider:
- Initial assessment: Expect to spend a few weeks undergoing diagnostic tests and evaluations to create a tailored treatment plan.
- Treatment Duration: Depending on the type of therapy, treatment can range from a few weeks to several months, with regular follow-ups to monitor progress.
- Recovery Time: Full recovery may take anywhere from a few weeks to over a year, especially if surgery is involved.
As for outcomes, it’s essential to set realistic expectations. While many patients experience significant improvements, the extent of recovery can vary widely. Here’s a simple overview of what you might anticipate:
| Outcome | Timeframe | Likelihood |
|---|---|---|
| Improved mobility | 1-3 months | 70% |
| Reduced pain | 2-6 months | 80% |
| Return to daily activities | 3-12 months | 60% |
By discussing these aspects with your MSK specialist, you can gain a clearer understanding of what to expect, allowing you to stay focused on your recovery goals and actively participate in your treatment plan.
4) Are there any lifestyle changes or exercises you recommend that could complement my treatment and promote long-term health? Your specialist can provide valuable insights on how to integrate wellness into your daily routine
Incorporating lifestyle changes and specific exercises into your routine can significantly enhance your treatment and promote long-term health. Your specialist may suggest focusing on a balanced approach that includes nutrition, physical activity, and mental well-being. Here are some lifestyle adjustments to consider:
- Nutrition: Embrace a diet rich in whole foods,emphasizing fruits,vegetables,lean proteins,and healthy fats.Consider consulting a nutritionist for personalized meal plans.
- Hydration: Staying well-hydrated is crucial. Aim for at least 8 glasses of water daily to support overall health and bodily functions.
- Mindfulness Practices: Incorporate meditation or yoga into your routine to reduce stress and improve mental clarity.
- Regular Check-ins: Schedule routine follow-ups with your specialist to monitor your progress and adjust your plan as needed.
When it comes to exercise, a tailored program can be instrumental in your recovery and maintenance.Here’s a simple table outlining some recommended activities:
| Activity | Duration | Benefits |
|---|---|---|
| Walking | 30 minutes, 5 times a week | Improves cardiovascular health and boosts mood |
| Strength Training | 20 minutes, 2-3 times a week | Builds muscle and enhances metabolism |
| Stretching | 10 minutes daily | Increases versatility and reduces injury risk |
| Swimming | 30 minutes, 2-3 times a week | Low-impact exercise that improves endurance |
Always consult with your specialist before starting any new exercise program to ensure it aligns with your treatment goals and physical capabilities. By integrating these lifestyle changes and exercises, you can pave the way for a healthier future.
5) How will we measure progress during my treatment, and what signs should I look for that indicate improvement or the need for a change in strategy? Clear benchmarks can help you stay focused and understand the effectiveness of your treatment plan
Understanding how progress will be measured during your treatment can empower you to actively participate in your care. Discuss with your MSK specialist the specific metrics that will be utilized to gauge your improvement. These could include pain levels, mobility assessments, or functional tests. Set clear benchmarks, such as achieving a certain level of pain reduction or completing specific physical tasks, to help you stay focused on your goals. Regular check-ins with your healthcare team will ensure that you’re on the right track and allow for timely adjustments if necessary.
Along with clinical assessments, be aware of subjective signs that indicate your condition is improving or may require a change in strategy. Look for improvements in your daily activities, such as:
- Increased energy levels
- Enhanced range of motion
- Better sleep quality
- Improved mood and mental clarity
Conversely, if you experience a plateau or worsening symptoms, it’s crucial to communicate these changes with your specialist. Keeping a journal of your experiences can be an invaluable tool in tracking these signs and discussing them during your appointments.
to sum up
As we wrap up our exploration of the five essential questions to ask your musculoskeletal (MSK) specialist,it’s clear that effective communication is the cornerstone of your care journey. By arming yourself with these inquiries, you empower not only your understanding but also your collaboration with your healthcare provider.Remember, your health is a partnership, and asking the right questions can pave the way for better outcomes and a clearer path to recovery.
So, the next time you step into your appointment, take a deep breath, and let these questions guide your conversation. Your body deserves the best care, and being informed is the first step toward achieving it. Here’s to taking charge of your health—one question at a time!







Leave a Reply
Want to join the discussion?Feel free to contribute!